What Is Iliotibial Band Syndrome?
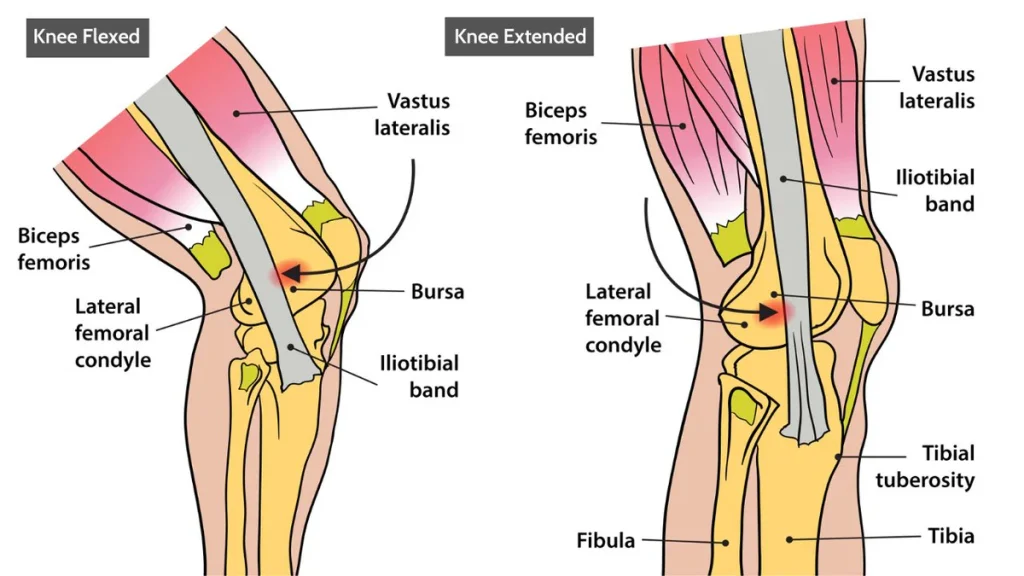
Iliotibial Band Syndrome (ITBS) is an overuse injury of the connective tissue that runs along the outside of the thigh, from the hip to the shin. The iliotibial (IT) band becomes tight or inflamed, causing pain on the outer side of the knee, especially during activities like running, cycling, or climbing stairs.
This condition is common in athletes, particularly runners, and is one of the leading causes of lateral knee pain.

What Causes Iliotibial Band Syndrome?
ITBS is caused by repetitive friction between the IT band and the outer part of the femur (thigh bone), known as the lateral femoral epicondyle. Common contributing factors include:
- Overuse from repetitive activities (like long-distance running or cycling)
- Tight or stiff IT band
- Weak hip or gluteal muscles
- Improper training techniques (sudden increases in distance or intensity)
- Running on uneven surfaces or downhill
- Worn-out or inappropriate footwear
- Poor biomechanics – like flat feet or leg length differences
Who Is at Risk for ITBS?
ITBS can affect anyone but is more common in:
- Long-distance runners and sprinters
- Cyclists
- Hikers and walkers
- Athletes who train on uneven terrain
- Individuals with tight muscles, poor posture, or imbalanced strength
- People with structural issues such as bowed legs, flat feet, or weak hip stabilizers
What Are the Symptoms of Iliotibial Band Syndrome?
The most common symptom is pain on the outside of the knee, particularly:
- During or after running or repetitive knee movement
- When walking downstairs or downhill
- With prolonged sitting or bending of the knee
- Sometimes accompanied by a clicking or snapping sound over the knee
- Tenderness or tightness along the outside of the thigh
Pain often worsens with continued activity and improves with rest.
How Is Iliotibial Band Syndrome Diagnosed?
Diagnosis is mainly clinical, based on symptoms and physical exam. Tests may include:
- Physical examination – tenderness along the IT band and pain when flexing the knee
- Ober’s test or Noble compression test – used to assess IT band tightness and irritation
- Imaging (rarely needed) – X-rays or MRI may be ordered to rule out other causes of knee pain, such as meniscus tears or arthritis
How Is Iliotibial Band Syndrome Treated?
Treatment aims to reduce inflammation, relieve pain, and correct the underlying cause. Common approaches include:
- Rest – avoid or reduce aggravating activities
- Ice therapy – apply ice packs to the outer knee to reduce swelling
- Anti-inflammatory medications – such as ibuprofen or naproxen
- Physical therapy – focusing on stretching the IT band and strengthening hip and glute muscles
- Foam rolling or massage therapy – to release tension in the IT band
- Correcting biomechanics – through custom orthotics or gait analysis
- Gradual return to activity – once pain has resolved and strength is restored
In rare, severe cases that don’t respond to conservative treatments, corticosteroid injections or even surgery may be considered.
Can Stretching and Exercises Help?
Yes, targeted stretching and strengthening exercises are key to recovery and prevention:
- IT band stretches – such as standing or seated cross-leg stretches
- Hip strengthening – clamshells, side leg raises, and bridges
- Foam rolling – on the IT band, quads, and glutes
- Core stability exercises – to improve alignment and posture
- Balance and mobility training – to improve coordination and lower body control
These exercises can relieve tightness and prevent recurrence.
Can ITBS Be Prevented?
Prevention focuses on proper training habits and maintaining good biomechanics:
- Warm up before and stretch after exercise
- Gradually increase workout intensity or mileage
- Strengthen the hips, glutes, and core muscles
- Use proper footwear and replace worn-out shoes regularly
- Avoid running on slanted or uneven surfaces
- Cross-train to reduce repetitive stress on the knees
Regular stretching and body awareness are key to avoiding re-injury.
What Is the Outlook for People with ITBS?
With proper treatment and activity modification:
- Most people recover within a few weeks to a couple of months
- Early intervention leads to faster recovery and fewer complications
- Ignoring symptoms can prolong healing or lead to chronic pain
- Once resolved, strengthening and stretching can help prevent recurrence
Most athletes can return to their normal activities with no long-term issues.
When Should You See a Doctor?
You should consult a healthcare provider if you:
- Have persistent or worsening pain despite rest
- Experience swelling or redness around the knee
- Are unable to continue your usual activities
- Need help with rehab exercises or gait assessment
Early evaluation can prevent chronic injury and help ensure a safe return to activity.


