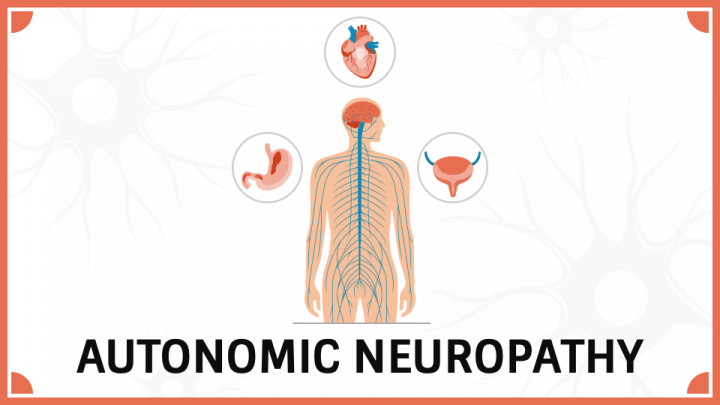
What Is Autonomic Neuropathy?
Autonomic neuropathy is a condition that affects the autonomic nervous system (ANS), which controls involuntary bodily functions such as heart rate, blood pressure, digestion, and sweating. When the nerves that manage these functions become damaged, it can lead to a variety of symptoms that impact several organ systems. The autonomic nervous system plays a crucial role in regulating bodily functions that happen automatically, like breathing, digestion, and regulating the body’s response to stress.
Autonomic neuropathy is often a complication of other medical conditions, especially diabetes, but can also be associated with other diseases, infections, toxins, and even genetic factors.
What Are the Causes of Autonomic Neuropathy?
Autonomic neuropathy can be caused by a variety of underlying conditions, including:
1. Diabetes
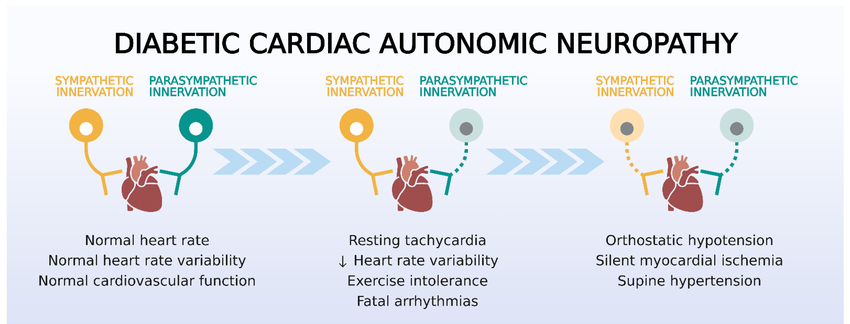
- Diabetic autonomic neuropathy is one of the most common causes. High blood sugar levels can damage the nerves over time, especially in people who have had diabetes for many years. The damage primarily affects the nerves controlling heart rate, blood pressure, digestion, and other involuntary functions.
2. Genetic Disorders
- Some inherited disorders, such as Familial Amyloid Polyneuropathy, can lead to autonomic neuropathy. These genetic conditions cause the buildup of abnormal proteins that damage the autonomic nerves.
3. Autoimmune Diseases
- Autoimmune diseases such as lupus and rheumatoid arthritis can also damage the autonomic nervous system. These conditions cause the immune system to mistakenly attack healthy nerve tissue.
4. Infections
- Certain infections, such as HIV, Lyme disease, and hepatitis C, can lead to nerve damage, including autonomic neuropathy.
5. Toxins
- Toxins from alcohol, drugs, or exposure to chemicals can also lead to nerve damage, including in the autonomic nervous system.
6. Nutritional Deficiencies
- Deficiencies in vital nutrients, such as vitamin B12, can cause nerve damage, potentially leading to autonomic neuropathy.
7. Other Causes
- Conditions like Parkinson’s disease, multiple system atrophy, and amyloidosis can also affect the autonomic nervous system, leading to neuropathy.

What Are the Symptoms of Autonomic Neuropathy?
Symptoms of autonomic neuropathy vary widely depending on which part of the autonomic nervous system is affected. Common symptoms include:
1. Cardiovascular Symptoms
- Low blood pressure (hypotension): Standing up may cause dizziness or fainting due to a drop in blood pressure.
- Tachycardia (rapid heart rate): Some people may experience an increased heart rate, especially after eating or standing up.
- Heart rate variability: Difficulty in regulating heart rate with stress, physical activity, or rest.
2. Gastrointestinal Symptoms
- Gastroparesis: A condition where the stomach empties too slowly, causing nausea, vomiting, bloating, and loss of appetite.
- Constipation: Difficulty passing stools, often due to impaired nerve control in the digestive system.
- Diarrhea: In some cases, autonomic neuropathy can cause frequent, unpredictable diarrhea.
3. Genitourinary Symptoms
- Bladder dysfunction: This can include difficulty emptying the bladder (urinary retention) or frequent urination.
- Sexual dysfunction: Autonomic neuropathy can affect sexual function, causing erectile dysfunction in men or vaginal dryness in women.
4. Sweating Dysfunction
- Excessive sweating (hyperhidrosis) or lack of sweating (anhidrosis) can occur due to impaired nerve function that controls sweat glands.
5. Other Symptoms
- Heat intolerance: Some people may feel excessively hot and sweaty or have difficulty regulating body temperature.
- Blurred vision: The autonomic nervous system controls pupil dilation, so damage may lead to problems with vision.
- Hypoglycemia unawareness: People with diabetes and autonomic neuropathy may not feel the symptoms of low blood sugar (hypoglycemia), increasing the risk of severe hypoglycemia.
How Is Autonomic Neuropathy Diagnosed?
Diagnosing autonomic neuropathy involves a thorough medical history and a variety of tests to evaluate how the autonomic nervous system is functioning. These tests may include:
- Physical Examination
- A doctor will assess your heart rate, blood pressure, and ability to sweat to look for signs of autonomic dysfunction.
- Tilt Table Test
- This test evaluates how your blood pressure and heart rate respond to changes in position, such as moving from lying down to standing up.
- Sweat Testing
- Special tests can measure how much you sweat in response to stimuli, helping to assess the function of sweat glands.
- Electrocardiogram (ECG)
- An ECG can assess how your heart rate and rhythm respond to various stimuli, which helps diagnose problems with autonomic regulation.
- Gastric Emptying Study
- This test measures how quickly food moves through the stomach, helping diagnose gastroparesis caused by autonomic neuropathy.
- Blood Tests
- Blood tests may be performed to check for underlying causes, such as diabetes, vitamin deficiencies, or infections that could be contributing to autonomic neuropathy.
How Is Autonomic Neuropathy Treated?
Treatment for autonomic neuropathy focuses on managing symptoms, treating the underlying cause, and improving quality of life. Common treatment strategies include:
1. Blood Sugar Control
- For individuals with diabetes, controlling blood sugar levels is crucial in slowing the progression of neuropathy and managing symptoms. Medications such as insulin or oral diabetes medications may be prescribed.
2. Medications
- Pain relievers: Over-the-counter pain relievers or prescription medications may be used to manage pain associated with autonomic neuropathy.
- Alpha-adrenergic agonists: These medications can help manage low blood pressure by constricting blood vessels and increasing blood pressure.
- Beta-blockers: These may be used to regulate heart rate and blood pressure.
- Anticholinergic drugs: These medications can help reduce excessive sweating and treat bladder dysfunction.
- Prokinetic agents: These drugs can help speed up gastric emptying and manage symptoms of gastroparesis.
3. Lifestyle Modifications
- Dietary changes: For people with gastroparesis, eating smaller meals more frequently and avoiding high-fat or high-fiber foods may be recommended.
- Physical therapy: Physical therapy may help with issues like balance, coordination, or muscle weakness due to autonomic dysfunction.
- Compression stockings: These can help manage symptoms of orthostatic hypotension (low blood pressure when standing) by improving blood circulation.
4. Supportive Therapies
- Cardiovascular support: In cases of blood pressure problems, medications or lifestyle changes may help support cardiovascular health.
- Biofeedback: This technique helps people learn to control physiological processes, such as heart rate and blood pressure, to reduce symptoms.
5. Treatment of Underlying Causes
- Treating the underlying condition causing autonomic neuropathy (such as diabetes, autoimmune disease, or nutritional deficiencies) is key to managing the condition.
Can Autonomic Neuropathy Be Prevented?
Prevention of autonomic neuropathy largely involves addressing risk factors and managing underlying conditions:
- Manage diabetes carefully: Keeping blood sugar levels within target ranges can prevent or slow the progression of diabetic autonomic neuropathy.
- Regular check-ups: Monitoring for early signs of autonomic dysfunction, especially in people with diabetes or other underlying conditions, can help detect issues early.
- Avoid toxins: Limiting alcohol consumption and avoiding exposure to harmful chemicals or medications that can cause nerve damage.
- Eat a healthy diet: Ensuring adequate nutrition, especially vitamin B12, to prevent neuropathy related to deficiencies.
- Exercise regularly: Physical activity can improve circulation and help manage blood pressure.


